A person with depression, or Major Depressive Disorder, may experience symptoms for more than two weeks.
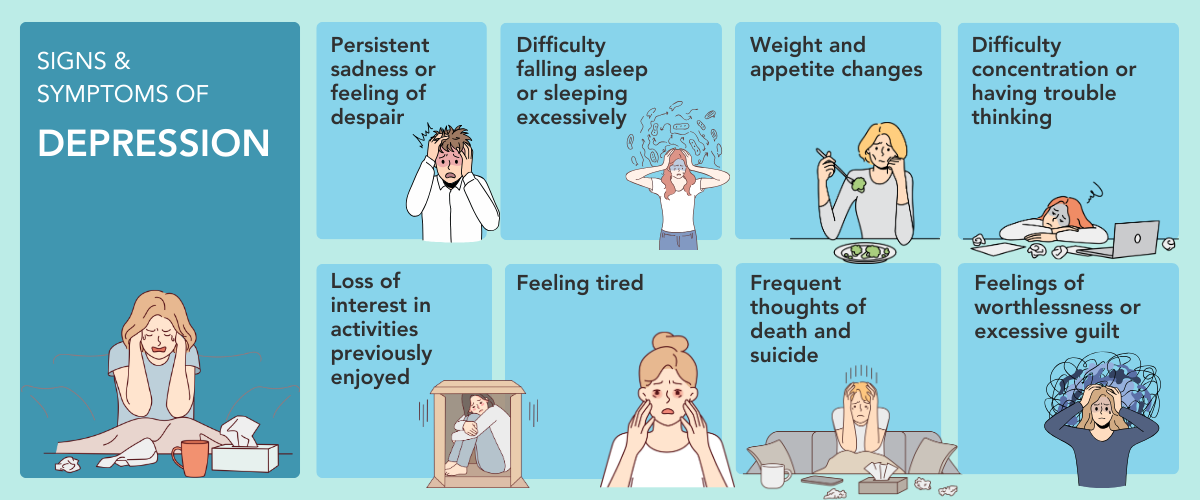
Signs and symptoms of depression include:
- Persistent sadness or feelings of despair
- Difficulty falling asleep, or sleeping excessively
- Changes in weight and appetite
- Difficulty concentrating or thinking
- Loss of interest in activities
- Feelings of worthlessness or excessive guilt
- Frequent thoughts of death or suicide
Dysthymia
Dysthymia is the chronic form of persistent, low-grade depression occurring over a continuous period. It does not have an episodic pattern as seen in Major Depressive Disorder. Research has shown that natural recovery from dysthymia is seen only in 10% of the cases. A five-year follow up study has shown that people who have untreated dysthymia developed Major Depressive Disorder (20%) and Bipolar II disorder(15%). The persistent symptoms of dysthymia can also affect their personal relationships and their work performance. Hence, professional help is required to address this under-diagnosed illness.
Holiday Blues
The “holiday blues” is a common phenomenon when people feel stressed or overwhelmed nearing the festive season, which starts towards year-end. The absence of close connections may be especially difficult to cope with during the season of gatherings. Societal expectations that surround the festive season and what it "should" feel like may create a sense of burden, as we find ourselves caught up in giving gifts as well as the constant socialising. People may feel a sense of loss and end up becoming withdrawn or isolated. The end of the year is also a time when people look back on their accomplishments in the past year and decide about resolutions for the new year. People who are highly self-critical or already depressed may feel worse during this time if they rate themselves lower in their accomplishments than others would, or blame themselves for not meeting their own or others' expectations.
Depression is highly treatable. When depression is recognised and treated, a person’s quality of life can be greatly improved. Treatment for depression is often approached from a multi-modal perspective.
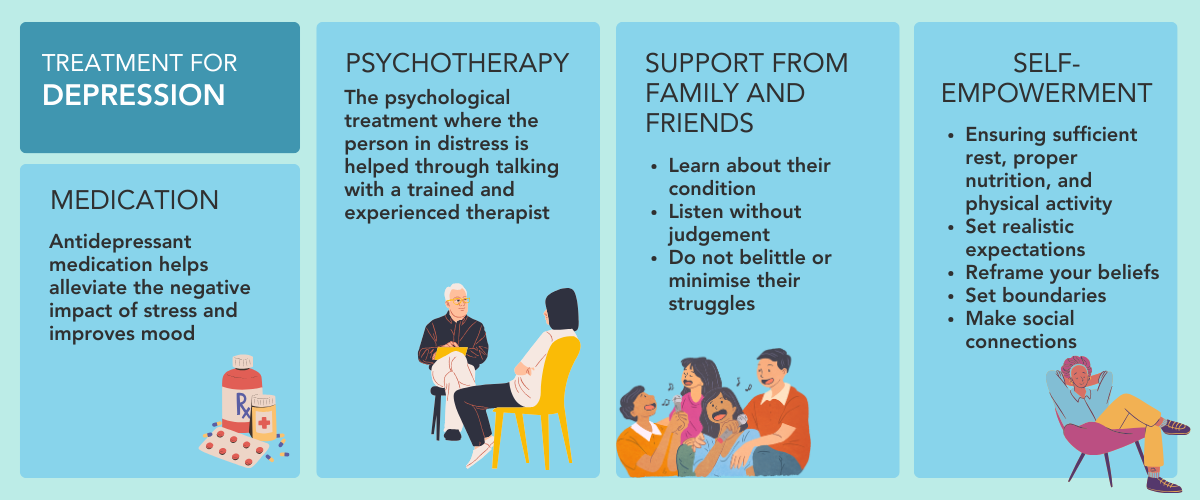
- Psychotherapy: Psychological treatment where the person in distress works with a therapist to develop goals and learn strategies
- Medication: Antidepressant medication can help improve mood
- Social support: Family and friends can learn about the condition and avoid belittling these struggles
- Self-empowerment: Persons with depression can care for their physical well-being through adequate rest and good diets. They may also reframe their unhelpful thoughts, and set boundaries and realistic expectations.